LAPAROSCOPIC SG DII
ROBOTIC, LAPAROSCOPIC SLEEVE GASTRECTOMY WITH DUODENOILEAL INTERPOSITION (SG DII) DIVERTED SLEEVE GASTRECTOMY WITH ILEAL INTERPOSITION (DSG II)
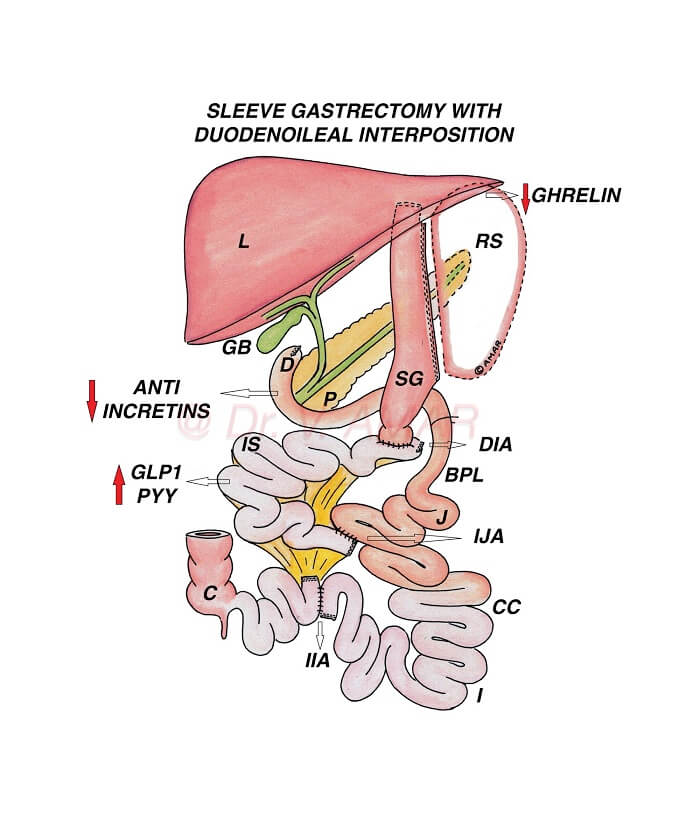
– It is a type of sleeve plus bypass combination surgery (Sleeve plus procedure) for the treatment of severe obesity and severe diabetes.
– It is a modification of biliopancreatic diversion with duodenal switch (BPD DS), with an additional anastomosis between distal ileum and jejunum.
– Procedure:
- Performed by robotic or laparoscopic method (By putting small holes over the tummy) using advanced high quality imported laparoscopic equipment and instruments.
- Up to 80% of the stomach is removed using high quality staplers and stapler guns to form a vertical sleeve.
- When the stomach is divided using staplers, it is stapled in three rows, sealed and cut simultaneously.
- The percentage of the removed stomach is relative but the capacity of the remaining gastric sleeve is 60 to 100 ml.
- Duodenum (First part of the small intestine) is divided.
- 170 cm segment of distal ileum (last part of the small intestine) is isolated and interposed between the divided first part of the duodenum and proximal jejunum.
– In India and Asia,
- Individuals suffering from severe obesity with the body mass index is ≥ 32.5 kg/m2 with co-morbid medical conditions such as type 2 diabetes.
- Individuals suffering from severe obesity with the body mass index is ≥ 37.5 kg/m2 even without any co-morbid medical conditions.
– In Western countries
- Individuals suffering from severe obesity with the body mass index is ≥ 35 kg/m2 with co-morbid medical conditions such as type 2 diabetes.
- Individuals suffering from severe obesity with the body mass index is ≥ 40 kg/m2 even without any co-morbid medical conditions.
– Weight loss is mainly due to physiological changes altering body energy balance.
– Because of these changes
- Appetite (Hunger) is reduced.
- Metabolic rate is increased.
- Energy expenditure is increased.
- ‘Fat mass’ is reset to a lower level.
- Fat starts melting as body doesn’t want to store large quantity of fat.
- You don’t eat large quantity of food as you start hating unhealthy foods.
– Physiological changes are high as undigested food rapidly enters the interposed ileal segment from from the first part of the duodenum.
– Diversion of the biliopancreatic juices contribute further to these physiological changes.
– Role of food restriction and malabsorption is secondary.
– Same physiological changes are responsible for type 2 diabetes remission.
- Insulin resistance is reduced.
- Insulin production is optimised to control blood sugars.
– Average excess weight loss is ~ 80 to 90%.
– Some may lose above average, even 100% of the excess weight loss but that number is less.
– For Example – If you are 50 kg excess weight, you lose approximately 40 to 45 kg on average. Some may lose all the extra 50 kg.
– Generally if your weight burden is less, you lose more percentage of excess weight and if your weight burden is more you lose less percentage of excess weight.
– Total weight loss percentage is ~ 35 to 40%.
– Average diabetes remission ~ 80 to 90%.
– It is necessary to follow lifestyle modifications to improve weight loss and diabetes remission and to prevent weight regain and diabetes recurrence.
– Results in long lasting and significant weight loss.
– Results in long lasting and effective diabetes remission.
– Physiological changes are relatively high in Sleeve with duodenoileal interposition as food directly enters interposed ileal segment compared to the standard Gastric sleeve (SG), Roux en y gastric bypass (RYGB) or mini gastric bypass – one anastomosis gastric bypass (MGB – OAGB), and Sleeve with bypass combination procedures such as Sleeve with duodenojejunal bypass (SG DJB), Sleeve with loop duodenojejunal bypass (SG LDJB), Sleeve with proximal jejunal bypass (SG PJB) or Sleeve with Jejunoileal anastomosis (SG JIA).
– Weight loss is more effective & long lasting after SG DII compared to the standard SG, RYGB or MGB – OAGB, and Sleeve with bypass combination procedures such as SG DJB, SG LDJB, SG PJB or SG JIA.
– Diabetes remission is relatively high & durable after Diverted sleeve with ileal interposition compared to the standard SG, RYGB or MGB – OAGB, and Sleeve with bypass combination procedures such as SG DJB, SG LDJB, SG PJB or SG JIA.
– Weight regain after Sleeve with duodenoileal interposition is low.
– Diabetes recurrence after Diverted sleeve with ileal interposition is low.
– SG DII has several advantages compared to RYGB and MGB – OAGB.
- There is no ‘at risk’ stomach remnant.
- Calcium and iron deficiency risk is low since first part of the duodenum is not bypassed
- Risk of dumping syndrome is less because of intact pylorus controlling food out put
- There is no risk of marginal ulcers
– Compared to BPD DS, risk of protein energy malnutrition, malabsorption and vitamin & mineral deficiencies is very low because common channel (intestine available for digestion and absorption) is very long.
– It is a very good procedure in individuals suffering from uncontrolled type 2 diabetes but BMI is < 30 kg/m2.
– SG DII is technically more advanced, complex and time taking compared to SG, RYGB and MGB – OAGB.
– It needs advanced laparoscopic surgical skills and training.
– There is loss of endoscopic access to biliary tract (Pathway connecting liver and small intestine).
– SG DII is less effective compared to Sleeve gastrectomy with loop gastroileal bypass (SG LGIB), Single anastomosis duodenoileal bypass with sleeve (SADI S) and BPD DS because bypassed small intestine (biliopancreatic limb) is relatively shorter.
– Some may lose below average. Inadequate weight loss ~ 05%. They may lose only 5 to 10 kg and stop losing further.
– Average weight regain ~ 15 to 25%.
– Diabetes recurrence after SG DII is ~ 25 to 35%.
– If anyone regains weight or if diabetes recurs after Sleeve with duodenoileal interposition, revision to Loop duodenal switch or Duodenal switch re-induce significant weight loss and diabetes remission.
– Risk of internal herniation and intestinal obstruction, but this is very rare as all the gaps in the mesenteric layers are closed carefully.
– It is very very safe procedure.
– It is a life saving surgery.
– Severe obesity and severe diabetes are dangerous.
– Bariatric and Metabolic surgeries are very safe.
– Complications are very rare. Even if they occur, they can be rectified.